Rethinking Obesity: Why BMI Still Matters
In recent discussions about obesity diagnosis, a growing number of experts are calling for an overhaul of how we understand and diagnose obesity, suggesting that Body Mass Index (BMI) is an outdated tool. However, before we throw out BMI entirely, it's worth considering why this simple measure has been a mainstay for decades and why it still holds significant value in the conversation about public health and obesity.
The Case for Keeping BMI
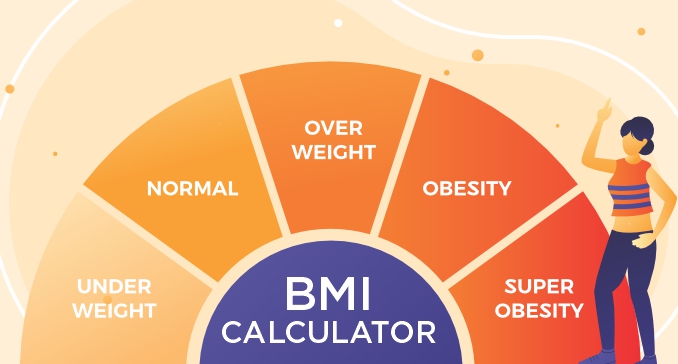
BMI, a straightforward calculation using weight and height, has been the go-to method for assessing obesity because of its simplicity and accessibility. While critics argue that it doesn't account for muscle mass, bone density, or fat distribution, it remains an effective screening tool for identifying populations at risk of obesity-related illnesses.
Take, for example, the United States, where obesity rates have soared over the past few decades. According to the Centers for Disease Control and Prevention (CDC), about 42% of American adults are classified as obese. This alarming statistic was largely identified using BMI. Critics may point to the limitations of BMI, but its role in highlighting such critical public health issues cannot be dismissed.
Moreover, BMI's simplicity makes it a practical tool for large-scale epidemiological studies. It allows researchers to track trends and correlations between obesity and various health outcomes across diverse populations. Without such a standardized measure, gathering comparable data would be a far more complex and costly endeavor.
Real-World Impact of BMI
In many real-world scenarios, BMI has proven its worth as a useful indicator of health risks. For instance, a study published in the New England Journal of Medicine found a strong correlation between high BMI and increased risk of heart disease, diabetes, and certain cancers. These findings have been instrumental in guiding public health policies and interventions aimed at reducing the burden of these diseases.
Consider the case of Japan, a country known for its relatively low obesity rates. Japan employs BMI as part of its national health guidelines and uses it to implement policies such as the "Metabo Law," which mandates waist measurements for people over 40. This approach has been credited with helping maintain Japan's status as a nation with one of the lowest obesity rates globally. It underscores how BMI, when used as part of a comprehensive health strategy, can be an effective tool for promoting healthier lifestyles.
A More Nuanced Approach
While BMI is not without its flaws, dismissing it entirely may be shortsighted. Instead, a more balanced approach that incorporates additional metrics alongside BMI could provide a fuller picture of an individual's health. For example, combining BMI with waist circumference or body fat percentage could help address the nuances that BMI alone cannot capture.
This integrated method has been successfully implemented in several health systems. In Australia, for example, the National Health and Medical Research Council recommends using both BMI and waist circumference to assess health risks related to obesity. This dual approach ensures that individuals who may be classified as overweight due to muscle mass, rather than fat, are not unfairly labeled as unhealthy.
The Risks of Overcomplicating Diagnosis
One potential pitfall of moving away from BMI is the risk of overcomplicating the diagnosis process. Introducing multiple metrics could create confusion among healthcare providers and patients alike, potentially leading to inconsistent diagnoses and treatment plans. Moreover, in resource-limited settings, the simplicity and cost-effectiveness of BMI make it a practical choice for initial screenings.
For developing countries struggling with both undernutrition and an emerging obesity epidemic, BMI offers a straightforward method to identify at-risk individuals without the need for expensive equipment or extensive training. Replacing BMI with a more complex set of criteria could hinder efforts to address the dual burden of malnutrition and obesity in these regions.
Embracing the Best of Both Worlds
Ultimately, while there is merit in exploring new ways to diagnose obesity, BMI should not be hastily discarded. Its simplicity, cost-effectiveness, and proven utility in public health make it a valuable tool in our ongoing battle against obesity. Instead of replacing BMI, we should aim to enhance it with additional measures that account for its limitations. By doing so, we can ensure that our approach to diagnosing and managing obesity is both comprehensive and accessible, empowering individuals and healthcare systems worldwide to make informed decisions about their health.
In this evolving conversation about obesity, it's crucial to remember that no single metric will provide all the answers. By embracing a multi-faceted approach that includes BMI, we can better address the complex nature of obesity and improve health outcomes for millions of people around the globe. Calculate your Body Mass Index with Free BMI Calculator.
Screen Studio
Beautiful Screen Recordings in Minutes. Screen Recorder producing high-impact videos automatically. Designed for macOS.


